
Managing lifestyle health changes with a depressed, anxious or stressed client
It’s not uncommon for those seeking to make health behaviour changes like losing weight, increasing activity and exercise, modifying diet or reducing alcohol consumption, to be simultaneously managing psychological health and wellbeing issues.
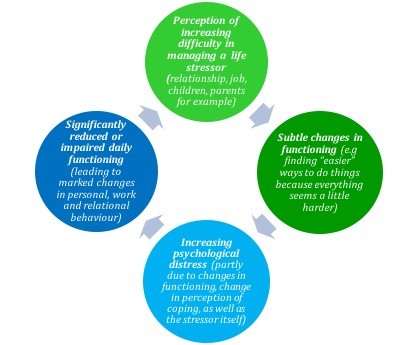
In fact, very often, our clients have become caught in a circular pattern which threatens to pull them into deep water, much like a whirlpool. It goes something like this:
- Perception of increasing difficulty in managing a life stressor (relationship, job, children, parents for example) ->
- Subtle changes in functioning (decreased commitment to exercise, finding “easier” ways to do things because everything seems a little harder, increased use of alcohol, less attention to meal planning, disturbed sleep) ->
- Increasing psychological distress (partly due to changes in functioning, change in perception of coping, as well as the stressor itself) ->
- Significantly reduced or impaired daily functioning (leading to marked changes in personal, work and relational behaviour) ->
- Perception of increasing difficulty in managing the life stressor (and other day to day events).
And on it goes. As a result of this cycle, many people end up feeling depressed, anxious or stressed, or a combination of all three. This often puts attention and commitment to lifestyle change at the very limits of reach. In general, chronic stress becomes distracting, chronic anxiety induces fear to act and chronic depression impairs motivation.
Trying to push ahead with health behaviour change in these circumstances is usually problematic. Because of the consequences noted above, clients struggle to achieve even small change or fail to notice it and quickly become demotivated and further challenged psychologically.
So, what can you do?
If you’re a primary care GP, refer your patient under a MHCP to a Psychologist and ideally one who is also familiar with health behaviour change and principles of lifestyle medicine. If there are other practitioners involved (such as dietitian or exercise physiologist) conducting a case conference at the outset of the referral to ensure everyone is on the same page is very helpful.
If you’re an allied health professional other than in mental health, get in touch with your client’s GP and discuss the situation with a view to the referral type described above.
If you’re a Psychologist or other mental health practitioner, the key is to engage your client in a discussion about this dilemma, outline the options you see and draw other options out of your client where possible. Being candid about the impact that psychological symptoms can have on attempts at health behaviour change can ease worries, reduce frustrations and make a contribution to getting your client on a helpful path to change. It also bolsters the therapeutic alliance – a key factor in recovery. In short, I’d be aiming to address the stress/anxiety/depression before resuming any significant health behaviour change work.
If you’re a “non-mental health” allied health professional working with the client to secure health behaviour change, the case conference is a great way to discuss how you can best support your client’s recovery from symptoms and signs of depression and anxiety before engaging in HBC.
Of course, in the same way that mental health and physical health are linked in the ways described above, it is also the case that improvements to physical health can favourably impact mental health, so focusing entirely on mental health to the exclusion of other lifestyle health until all mental health symptoms have remitted won’t be ideal.
In addition to the best practice guidelines I’ve linked to below, here are some other practice tips to assist your patients and clients to manage recovery from an episode of poor mental health:
- Convey confidence that the situation can be managed. This is important and frequently overlooked. The provision of realistic hope for clients has a measurable impact on treatment efficacy. Be candid, honest and confident.
- Do some reality checking of goals to ensure they’re achievable. A 0-10 scale is helpful here. Ask your client where they currently see themselves on the scale and identify what a ½ point increment would look like. Then reality-test this if necessary. People with high achieving and perfectionistic personality features will often overestimate a small change. Better to be frequently reaching small goals than struggling to reach a larger one.
- Help your client identify one or more people they can share their small successes with – this helps to reinforce change.
- Be alert for negative self talk (“I’m so stupid – I shouldn’t have done that”; “I’m hopeless at trying to exercise”). Challenge this respectfully and offer an alternative like “I fell back into an old habit yesterday but I have the tools to make small changes”.
- Highlight as much change as you can, no matter how small or insignificant it may seem. If your client got out of bed when they wanted just one day of the week, that may be one day more than the week before. If they stopped drinking alcohol two drinks before they usually might, that’s worth exploring.
For resources on best practice management of depression, anxiety and stress as recently revised by the RANZCP, you can follow this link1.
If you’re an APS member, the APS website has detailed practice guides for the treatment of depression and anxiety which can be found here2.
Simon Matthews is a Registered Psychologist, Fellow of the Australasian Society of Lifestyle Medicine, and Member of the Australian Psychological Society.
This article has been written for the Australasian Society of Lifestyle Medicine (ASLM) by the documented original author. The views and opinions expressed in this article are solely those of the original author and do not necessarily represent the views and opinions of the ASLM or its Board.



